FTM Phalloplasty and the Role of the Reconstructive Urologist
Reconstructive urology is a highly specialized field of urology that aims to restore both structure and normal function to the genitourinary tract.
The genitourinary tract—also called the genitourinary system, urogenital system, urogenital tract—is the system of the reproductive organs and the urinary system. The kidneys, bladder and urethra are parts of the genitourinary tract.
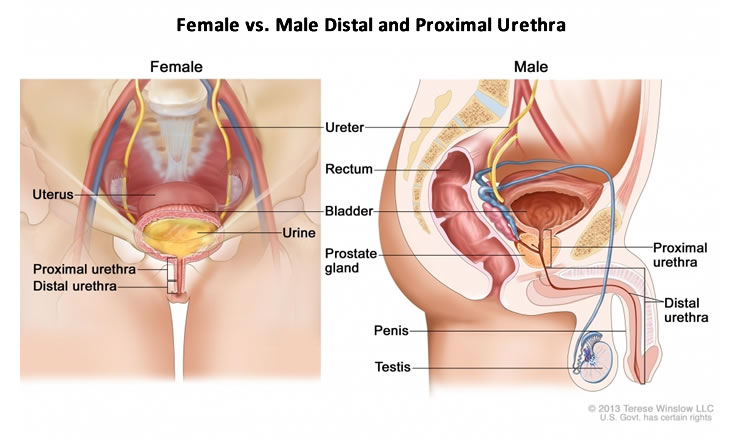
In FTM Phalloplasty procedures that include Urethroplasty (Urethral Lengthening), the genitourinary tract undergoes transformation: the urethra is extended by several inches, from the native urethral opening to the tip of the neophallus. This urethral "renovation" is a challenging aspect of Phalloplasty and can lead to complications, particularly urinary fistula (abnormal passageways) and urethral stricture (blockage).
When trans men experience conditions like incontinence or urinary obstruction after Phalloplasty, it can significantly affect quality of life. Post-operative urological complications can be managed by the original surgical team, or the patient can be referred to a Reconstructive Urologist.
The role of the Reconstructive Urologist is to diagnose patients with urinary conditions and provide a solution to restore urinary functions. Put more simply, Reconstructive Urologists are trained to tackle difficult urinary complications. With insurance companies covering Phalloplasty increasingly, and Reconstructive Urologists being called on to fix post-op complications, it's not surprising that transgender urology is a growing field.
Common urinary complications after FTM Phalloplasty include urethral strictures, fistulas, and abscesses. It's not uncommon to have more than one complication at the same time, which can delay and add complexity to a repair surgery.
 Dr. Dmitriy Nikolavsky is a Reconstructive Urologist at SUNY in Syracuse, New York with a special interest in transgender urology. He sees patients who have developed post-operative complications with the urethra after Phalloplasty (or Metoidioplasty). While many urinary fistulas will heal with conservative treatment that doesn't require surgery, Dr. Nikolavsky performs repair surgeries for more persistant fistulas using a fasciocutaneous groin flap or a labial fat pad flap harvested from the neoscrotum.1
Dr. Dmitriy Nikolavsky is a Reconstructive Urologist at SUNY in Syracuse, New York with a special interest in transgender urology. He sees patients who have developed post-operative complications with the urethra after Phalloplasty (or Metoidioplasty). While many urinary fistulas will heal with conservative treatment that doesn't require surgery, Dr. Nikolavsky performs repair surgeries for more persistant fistulas using a fasciocutaneous groin flap or a labial fat pad flap harvested from the neoscrotum.1
For stricture repair surgeries, there are a few different methods depending on the size and location of the stricture.2 Cutting out the stricture and closing it may be possible, but closure may need to be augmented by tissue taken from the inside of the cheek, or less commonly, remnants of vaginal tissue, or rectal tissue. Some difficult strictures require a two-stage approach. For complex strictures that are not correctable, a final option is to relocate the urethra to the perineum, behind the neoscrotum.
FTM Phalloplasty is a complex surgery that is fraught with potential complications, particularly with the urinary system. A Reconstructive Urologist can provide diagnosis and solutions for difficult urinary complications after Phalloplasty. It's recommended that all trans men undergoing Phalloplasty be aware of the Reconstructive Urologists closest to them, just in case a complication develops after surgery that requires urological repair.
Footnotes
1. Dmitriy Nikolavsky et al, "Management of Unfavorable Urologic Sequelae After Phalloplasty in Transgender Patients," in Gender Affirmation: Medical and Surgical Perspectives (Thieme, Dec 1, 2016.)
2. Dmitriy Nikolavsky et al.